Non-Alcoholic Fatty Liver Disease (NAFLD) is a condition where excess fat builds up in the liver without alcohol consumption being a contributing factor. Hepatology, which focuses on liver health, plays a significant role in understanding and managing NAFLD. Here is more information on the basics of NAFLD and the role of hepatology in its management:
Exploring Hepatology
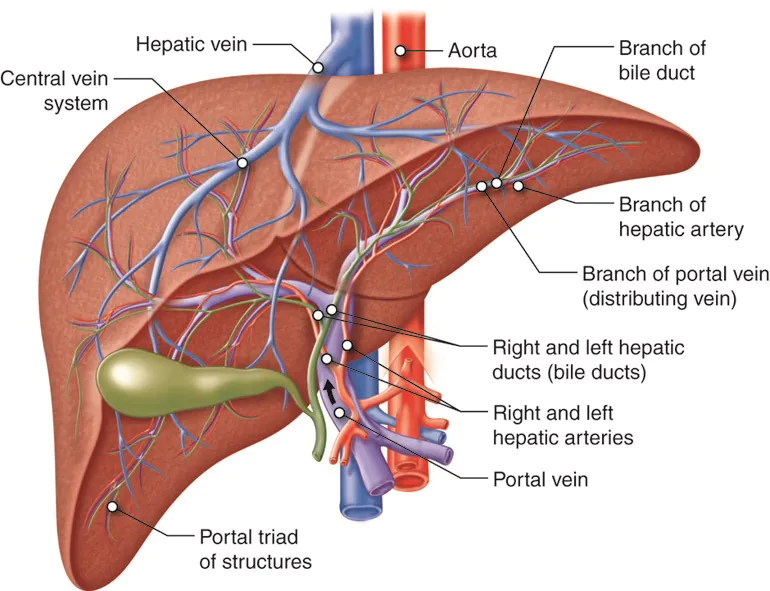
Hepatology, a specialized branch of medicine, focuses on understanding and managing liver-related conditions. Hepatologists play a role in addressing NAFLD by assessing the severity, monitoring progression, and guiding management strategies. Diagnosis and assessment involve evaluating liver fat levels, inflammation, and fibrosis.
This is done through diagnostic imaging, such as ultrasounds or elastography, and laboratory tests. In cases where advanced disease is suspected, a biopsy may be recommended.
Monitoring progression is another key aspect, as early identification enables specialists to track the condition and prevent complications. This often involves regular follow-ups with liver enzyme tests, imaging scans, or non-invasive fibrosis markers to monitor potential disease advancement.
For management, hepatologists work closely with patients to develop strategies tailored to their medical conditions. This may include addressing lifestyle factors that impact liver health and collaborating with other specialists.
Understanding NAFLD
NAFLD refers to a spectrum of liver conditions caused by fat accumulation in individuals who drink little to no alcohol. It is commonly divided into two categories:
- Non-Alcoholic Fatty Liver (NAFL): A milder condition where fat accumulates in the liver without causing significant inflammation or damage.
- Non-Alcoholic Steatohepatitis (NASH): A more severe condition characterized by liver inflammation and potential liver damage, which can lead to scarring (fibrosis) and potentially cirrhosis over time.
NAFLD often occurs alongside metabolic risk factors such as obesity, type 2 diabetes, high cholesterol, and high blood pressure. It is typically diagnosed through imaging tests, blood work, or, in select cases, liver biopsy. Although this condition can remain asymptomatic for years, progression can pose risks to the liver and overall health.
Adjusting Lifestyle Factors
Maintaining liver health can involve a range of lifestyle changes and preventive measures. While individual recommendations may differ, these steps often align with general well-being:
- Dietary Adjustments: A balanced diet rich in vegetables, fruits, whole grains, and healthy fats can help reduce liver fat levels. Reducing added sugars and saturated fats also aids in managing factors that contribute to NAFLD.
- Physical Activity: Engaging in regular physical activity helps regulate body weight while improving insulin sensitivity. Aerobic exercises, strength training, or even daily walks can contribute to an optimal metabolic state.
- Addressing Comorbidities: Managing conditions such as diabetes, obesity, and high cholesterol supports overall health while reducing strain on the liver. Routine medical consultations enable ongoing prevention.
- Avoiding Liver Stressors: Limiting the use of substances that stress the liver, such as alcohol or certain medications, promotes resilience over the long term.
Individuals with concerns related to their liver health may benefit from discussing potential strategies with a hepatologist or primary care provider.
Find a Gastroenterologist
With NAFLD becoming increasingly common due to metabolic risk factors, hepatology continues to advance the understanding and management of this condition.
From accurate diagnoses to personalized care plans, hepatologists play a key role in helping individuals prioritize liver health. Through informed lifestyle changes and proactive monitoring, many can take meaningful steps to support their liver and overall well-being.
Recommended Articles




Leave a Reply